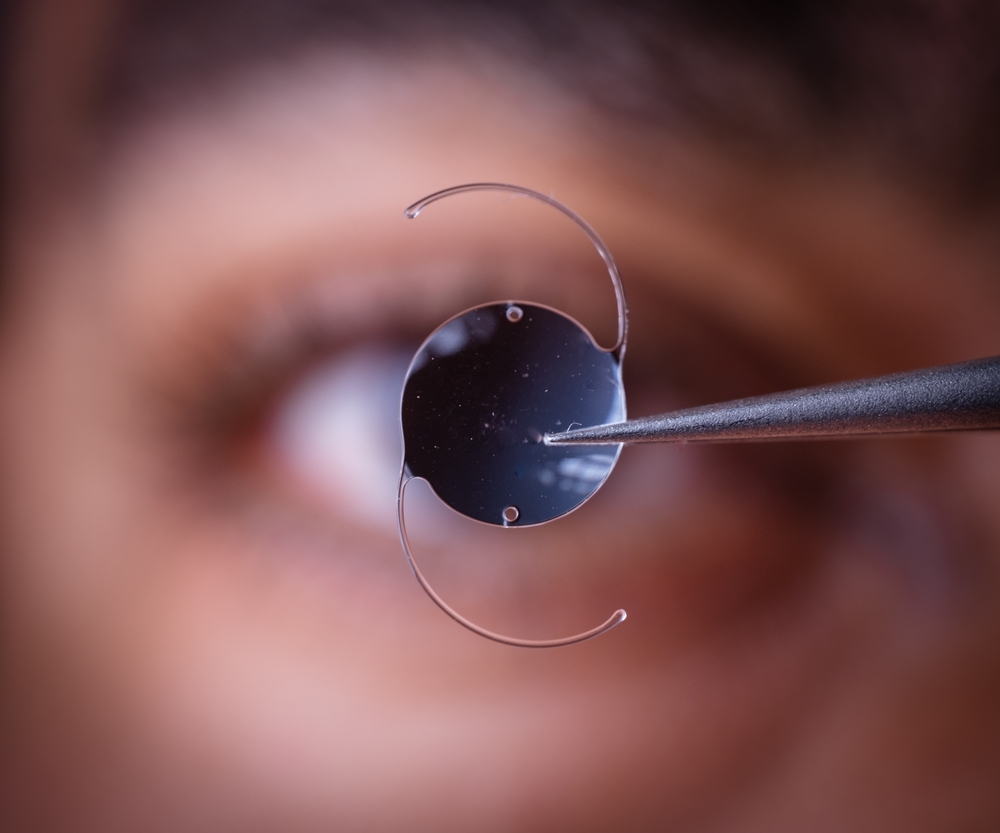
Vision is one of our most precious senses, and it’s no surprise that innovations in ophthalmology are of immense significance to many. In particular, Intraocular Lenses (IOLs) are the unsung heroes of modern eye surgery, especially in the context of cataract treatment. Cataract surgery has become a restorative procedure and an opportunity to upgrade your vision.
However, despite the sophistication of surgical techniques, the effectiveness and safety of these procedures are significantly influenced by a rather unassuming component – the IOL material. Let’s dive deeper into IOL materials, the importance of the material, and some safety considerations you must know.
Introduction to IOL Materials
The choice of IOL material is pivotal in determining the long-term results of cataract surgery. Factors such as optical clarity, biocompatibility, flexibility, refractive index, and anterior chamber stability are just a few among a host of considerations. Let’s delve into the three primary materials used in IOL manufacturing – PMMA, Acrylic, and Silicone – and understand what makes each unique.
The Significance of Material Selection
IOL surgeries are not one-size-fits-all. The patient’s age, lifestyle, and ocular health should influence the material selection. Understanding the features and differences between materials is the first step in personalized cataract care.
A Trio of Materials: PMMA, Acrylic, and Silicone
Each of these materials has its properties that can affect vision outcomes and patient safety post-cataract surgery. But what are these properties, and how do they translate into the real world?

PMMA IOLs
Historically, IOLs were made of PMMA, a rigid yet reliable polymer. In fact, the first intraocular lens implanted into a human was made of this material. Although newer materials have overshadowed PMMA in the last few decades, there are still scenarios where PMMA remains the material of choice.
Characteristics and Legacy
PMMA IOLs have been used since the 1940s, providing exceptional optical outcomes. Their main draw is the optical clarity and the ability to focus light precisely, which is ideal for some patients with specific needs.
Biocompatibility and Safety
The inert nature of PMMA makes it one of the safest materials used in surgical implants. The immune system doesn’t recognize PMMA as foreign, which minimizes the risk of inflammation and adverse reactions.
Acrylic IOLs
With advancements in medical-grade plastics, acrylic IOLs have emerged as a versatile choice, suitable for a wide range of patients and conditions. Their flexibility opens doors to various surgical techniques.
Features and Advancements
Highly modified acrylics offer outstanding optical clarity and are suitable for micro-incision cataract surgery, reducing the surgical footprint and leading to rapid healing.
Biocompatibility and Safety Considerations
Acrylic IOLs are designed to mimic the natural lens in material characteristics and biocompatibility, aiming for comfort and longevity within the eye.
Silicone IOLs
Silicone IOLs bring flexibility into the limelight, especially in accommodating IOLs designed to emulate the natural lens and enable focusing at various distances.
Properties and Flexibility
Silicone’s unique properties make it possible to create lenses that can change shape within the eye, providing a dynamic range of vision suitable for presbyopia correction.
Biocompatibility and Long-term Safety
Silicone IOLs, when first introduced, faced some concerns regarding capsular opacification, but material improvements have addressed this, ensuring excellent biocompatibility and long-term safety.
Comparing Biocompatibility Across Materials
Ensuring the biocompatibility of Intraocular Lenses (IOLs) is crucial for patient safety and long-term satisfaction. Several factors contribute to the biocompatibility of IOL materials, each playing a significant role in the body’s response to the implanted lens. It is vital to understand these factors to provide IOLs that are optimal in their refractive properties and harmonious with the patients’ ocular environment.

Tissue Reactions
One key factor in biocompatibility is how much a material causes inflammatory tissue reactions. Ideally, IOL materials should not incite a significant immune response, reducing the risk of postoperative inflammation or infection, which could compromise visual outcomes.
Capsular Opacification Prevention
Another important factor is the material’s ability to minimize postoperative capsular opacification. This common complication can affect vision, and materials that resist the formation of lens epithelial cells on the capsule can improve patients’ long-term clarity of vision.
Uveal and Corneal Biocompatibility
Tolerability by uveal and corneal tissues is also a defining factor in the biocompatibility of IOLs. Materials that exhibit poor uveal biocompatibility can result in pigment dispersion, while those that are unfavorable to the cornea might lead to endothelial cell loss over time.
Calcification Resistance
Resistance to calcification is an essential biocompatibility factor, as calcification on the IOL can lead to decreased vision and the need for IOL exchange. Materials that display a natural resistance to calcification ensure the clarity and longevity of the IOL.
Compatibility with Surgical Procedures
Lastly, the biocompatibility factor extends to how well IOL materials interact with specific surgical techniques and adjunctive devices or medications used during surgery. Materials should maintain integrity and not be prone to degradation or adverse interactions that could compromise the surgical outcome.
Choosing the Right IOL Material: Factors to Consider
The path to the right IOL material is not just picking the latest or the most technologically advanced. It should be a thoughtful process rooted in patient-centric decision-making.
Patient-Specific Needs and Ocular Health
- Refractive Error and Prescription: Consideration of the patient’s refractive error and prescription is crucial in determining the appropriate IOL power and type for optimal visual outcomes.
- Astigmatism Correction: Addressing astigmatism is essential, and certain IOLs are designed to correct or mitigate astigmatism, offering improved clarity of vision.
- Lifestyle and Activities: Understanding the patient’s lifestyle and activities helps tailor the choice of IOL material to meet specific visual demands, such as those of an active or passive lifestyle.
Improve Your Vision with Eye Care Professionals
IOL materials are the silent actors in the grand production of cataract surgery. We can foster better patient outcomes by understanding and appreciating the granular differences in these materials.
At Eye Care Professionals, we pride ourselves on staying at the forefront of technological advances in the field while maintaining our commitment to patient care. Our experienced and knowledgeable team is dedicated to providing personalized treatment plans that cater to each patient’s needs, ensuring they receive the best possible results.
We understand the importance of choosing the right IOL material. Also, we will work closely with you to determine the most suitable option for your ocular health and lifestyle. With our expertise and state-of-the-art technology, we can help you improve your vision and enhance your overall quality of life. Contact us today to schedule a consultation.