Diabetic retinopathy is a diabetes complication that affects the eyes. It’s caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina). Initially, diabetic retinopathy may cause no symptoms or only mild vision problems. However, it can eventually lead to blindness.
This article provides a comprehensive look at the signs and symptoms of this eye condition, emphasizing the critical role of early detection and treatment. Understanding these can lead to timely medical interventions that can significantly alter the course of this disease.
Importance of Early Detection and Treatment
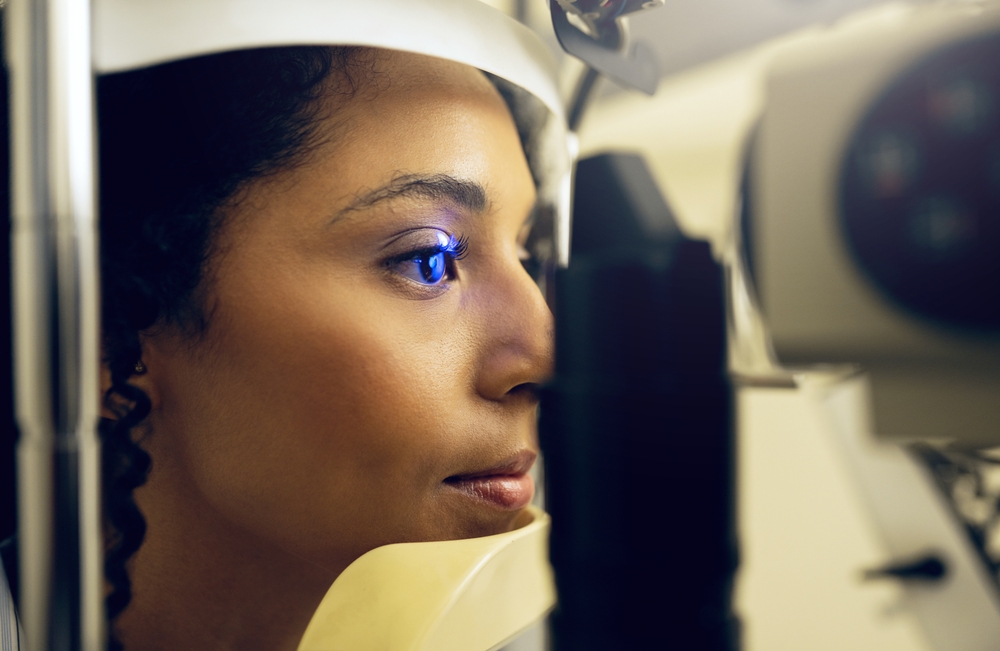
Early detection and treatment of diabetic retinopathy are crucial in preventing irreversible damage to the retina, which can lead to severe vision loss or blindness. Regular diabetic retinopathy exams are essential for anyone with diabetes.
These exams help catch signs of retinopathy early when it is most treatable and can prevent further deterioration of vision. Maintaining a schedule of regular eye exams allows healthcare providers to monitor changes over time and adjust treatment plans as needed. This proactive approach is vital for managing diabetes effectively and preserving eye health.
What is Diabetic Retinopathy?
Diabetic retinopathy is a condition that results from prolonged high blood sugar levels due to diabetes, leading to damage in the retina’s blood vessels. Over time, this damage can impair vision and lead to vision loss if not addressed properly through medical intervention. The retina is crucial for capturing visual images, which are then transmitted to the brain for interpretation. When the blood vessels in the retina are damaged, they can leak fluid or bleed, causing the retina to swell and form deposits. This can distort and blur vision, making everyday tasks increasingly difficult.
How Does Diabetes Affect Blood Vessels in the Retina?
Diabetes affects the body’s ability to use and store sugar properly, leading to high blood sugar levels. This excess sugar in the blood can damage the tiny blood vessels in the retina, the part of the eye that senses light and sends images to your brain. This damage can cause the vessels to leak or become blocked, interfering with vision over time. Over prolonged periods, this vascular damage can progress, resulting in the retina receiving less oxygen and nutrients. The eye may attempt to grow new blood vessels as a defense mechanism.
However, these new vessels are often fragile and prone to leakage, further complicating the health of the retina and exacerbating vision problems. This cycle of damage and inadequate repair underscores the critical need for diabetes management and regular eye examinations to detect and mitigate these changes early.
Causes and Risk Factors
Understanding the causes and risk factors for diabetic retinopathy can help manage and potentially prevent this condition. Detecting diabetic retinopathy signs early is crucial for timely intervention, which can significantly affect the disease’s progression and the patient’s quality of life. Key risk factors include:
Diabetes: Type 1
Type 1 diabetes typically starts early in life as an autoimmune disease where the immune system attacks insulin-producing cells in the pancreas. Those with Type 1 diabetes need insulin injections to manage blood sugar levels. Persistent high blood sugar can increase the risk of developing diabetic retinopathy, highlighting the importance of strict blood sugar control.
Diabetes: Type 2
Type 2 diabetes commonly develops in adults and is often associated with obesity and a sedentary lifestyle. This form of diabetes results from the body’s ineffective use of insulin. The risk of diabetic retinopathy increases if Type 2 diabetes is not well-managed, making regular medical oversight crucial for preventing complications.
Duration of Diabetes
The length of time a person has been living with diabetes correlates strongly with the risk of developing diabetic retinopathy. The longer someone has diabetes, the higher the likelihood of vascular damage in the retina due to prolonged exposure to high blood sugar levels.
Poor Blood Sugar Control
Maintaining blood sugar levels within a target range is critical for preventing or delaying the onset of diabetic retinopathy. Poor blood sugar control can accelerate the progression of retinopathy, making rigorous diabetes management essential.
High Blood Pressure
High blood pressure, or hypertension, is another significant risk factor for the development of diabetic retinopathy. Hypertension exacerbates the damage to the delicate blood vessels in the retina, further contributing to the complications associated with diabetic retinopathy. Managing blood pressure is, therefore, a critical component of treatment and prevention strategies for diabetic retinopathy.
Protect Your Vision Health in Reno Today
Diabetic retinopathy is a serious condition, but early detection and proper management can safeguard your vision and overall well-being. Trust Eye Care Professionals for expert care in Reno, NV. Contact us today to schedule your diabetic retinopathy exam and protect your eye health!