There is a broader trend in eye health toward precision, personalization, and long-term vision preservation. These principles are very much applied to the treatment of glaucoma, a leading cause of blindness that affects over 76 million people globally.
Understanding Glaucoma
Brief Overview of Glaucoma and Its Impact on the Optic Nerve
Glaucoma is not a single disease, but rather a group of conditions that cause progressive damage to the optic nerve—the communication highway between your eye and brain. This damage occurs gradually and is often painless, which means many people do not realize they have glaucoma until vision loss has already occurred. Left untreated, glaucoma can eventually lead to complete blindness, making early awareness and intervention critical for preserving eye health.
The Role of Intraocular Pressure (IOP)
Increased intraocular pressure (IOP) is the most common and controllable risk factor for glaucoma, typically resulting from fluid buildup in the eye due to poor drainage. As pressure builds, it compresses and slowly deteriorates the optic nerve, causing irreversible visual field loss over time. By maintaining a healthy IOP through medications, surgery, or implants, eye care professionals can slow or even halt disease progression in many cases.
Why Early Detection and Effective Treatment Are Crucial
Glaucoma is known as the “silent thief of sight” because its damage progresses without noticeable symptoms until vision is already compromised. Regular eye exams are essential, particularly for individuals over 40 or those with a family history of the condition. With early detection, patients have access to a wide array of modern treatments designed to control pressure and protect long-term vision before significant damage occurs.
Advancements in Medical Therapies
Sustained-Release Drug Delivery Systems
One of the biggest challenges in glaucoma care is patient adherence to daily eye drop regimens, which are often inconvenient and easy to forget. Sustained-release drug delivery systems provide a breakthrough by releasing medication over weeks or months with a single application. This not only improves long-term IOP control but also reduces patient error and increases overall treatment effectiveness.
Implants: Biodegradable Implants for IOP Control
Among the most promising options is the iDose implant, a tiny device placed inside the eye that slowly releases medication over time. Biodegradable options like the Bimatoprost and Travoprost implants dissolve naturally after delivering the therapeutic dose, minimizing the need for removal or additional procedures. These implants are particularly valuable for patients who struggle with compliance or require steady IOP reduction without fluctuation.
Punctal Plugs: Drug Delivery Through Tear Ducts
Punctal plugs are tiny devices inserted into the tear ducts to slow the drainage of tears and deliver medication over time, helping to maintain therapeutic levels in the eye. Unlike traditional drops, punctal plugs offer passive delivery that doesn’t depend on patient discipline. This system supports more consistent IOP management and is well-suited for individuals seeking lower-maintenance treatment options.
Benefits: Improved Adherence and Consistent Control
One major advantage of these modern therapies is the increased adherence they offer, particularly through the use of iDose TR. With reduced dosing frequency and longer-lasting effects, patients experience less burden and more consistent IOP regulation. These methods are transforming glaucoma care from a daily challenge into a simplified, long-term management strategy.
Breakthroughs in Surgical Interventions
Minimally Invasive Glaucoma Surgery (MIGS)
MIGS procedures are designed to reduce eye pressure using micro-incisions and miniature devices, offering a safer alternative to more aggressive surgical options. These surgeries aim to restore or enhance the eye’s natural fluid drainage mechanisms with minimal tissue disruption. As a result, patients experience fewer complications, faster healing, and shorter downtime.
Less Invasive Than Traditional Surgeries
Unlike trabeculectomy or tube shunt procedures, MIGS avoids extensive manipulation of eye tissues, reducing risks like infection, scarring, or long-term inflammation. This makes it an ideal first surgical option for early-to-moderate cases. Many patients who undergo MIGS report improved quality of life with fewer post-operative restrictions and complications.
Quicker Recovery Times and Fewer Risks
Because of the less invasive nature of MIGS, patients often resume normal activities within days instead of weeks. This accelerated recovery timeline, combined with fewer surgical risks, helps glaucoma patients maintain both vision and lifestyle. The effectiveness of these procedures continues to grow as new techniques and tools are developed.
Micro-Stent Implants: Improving Fluid Drainage
A major component of MIGS is the use of glaucoma implants, like the iStent, Hydrus Microstent, and Xen Gel Stent. These micro-sized stents are inserted into drainage canals within the eye to improve outflow of aqueous humor, effectively lowering IOP without damaging surrounding structures. Their safety and precision have made them a popular choice in early surgical intervention.
Often Combined with Cataract Surgery
Patients who suffer from both glaucoma and cataracts often benefit from combining MIGS with cataract surgery, which allows both issues to be treated simultaneously. This dual-procedure approach offers a single recovery period and streamlined care plan. It’s an efficient option that significantly enhances vision and eye pressure control for aging patients.
Advanced Laser Technologies
Selective Laser Trabeculoplasty (SLT)
SLT is a non-invasive laser treatment that targets the trabecular meshwork, stimulating it to drain fluid more efficiently. This painless outpatient procedure is quick to perform and has minimal side effects, making it a preferred first-line therapy for many newly diagnosed patients. It can be repeated if necessary and works well for those seeking a drug-free approach.
Increasingly Used as a First-Line Treatment
Recent studies like the LiGHT trial have shown that SLT can be as effective as daily eye drops in controlling IOP for certain patients. As a result, it is gaining popularity as a starting point for glaucoma therapy rather than a last resort. This evidence-based shift in treatment guidelines is improving long-term outcomes and patient satisfaction.
Micropulse Laser Therapy and Endoscopic Cyclophotocoagulation (ECP)
Other laser-based options include Micropulse Laser Therapy, which delivers energy in short bursts to avoid damage. At ECP, our surgeons use an endoscope to target ciliary body tissue precisely. Both treatments offer customized IOP reduction while preserving healthy structures in the eye. These innovations continue to expand the non-invasive options available for managing glaucoma effectively.
Emerging Technologies and Future Directions
Artificial Intelligence (AI) and Telemedicine
Technology is also revolutionizing diagnosis and long-term management through the integration of AI and remote monitoring. These systems analyze large volumes of data quickly, helping clinicians detect subtle changes that could indicate early-stage glaucoma.
AI-Powered Screening Tools
AI algorithms are now used to scan retinal images and detect optic nerve changes long before human doctors can. This enables earlier diagnosis and intervention, particularly in at-risk populations. Screening tools powered by AI can be deployed in both clinical and community settings, increasing access to preventative care.
AI Integration with OCT Imaging
By pairing AI software with Optical Coherence Tomography (OCT), eye care providers can better assess optic nerve fiber health. This dual approach provides a more detailed view of nerve integrity and disease progression. As AI continues to evolve, its role in treatment planning and monitoring will become even more vital.
Telemedicine for Remote Monitoring and Access
Telehealth platforms allow glaucoma patients to receive expert care and follow-up consultations without needing frequent in-person visits. This is particularly helpful for rural patients or those with mobility issues. As these systems improve, remote IOP monitoring and AI-assisted diagnostics may become a standard part of glaucoma care.
A Brighter Outlook for Glaucoma Patients in Reno, NV
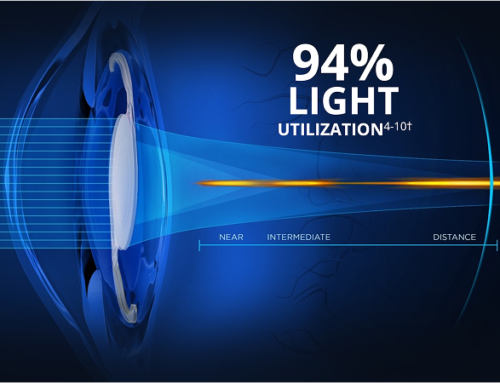
The future of glaucoma treatment is full of promise, powered by innovations that put control back into the hands of patients and providers. From light adjustable lenses cataract surgery that allows post-op vision personalization to the precision of iDose TR advanced glaucoma implants, the field is transforming rapidly. With these tools, we are not only treating glaucoma—we are preserving vision, independence, and quality of life for the long term.
Take control of your vision with light adjustable lenses cataract surgery. Contact Eye Care Professionals to schedule a consultation and experience personalized post-surgery results like never before.